How to Get the Greatest Return From Your Dry Eye Patients
By Mary Hollis Stuck August 05, 2021
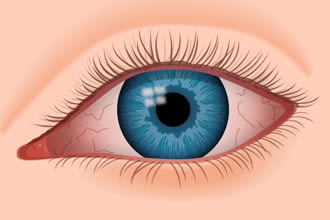 Dry Eye Syndrome is an incredibly common problem among patients of all ages. Doctors regularly treat and prescribe patients complaining of a burning, gritty feeling in their eyes, which can be caused by a reduction of lacrimal secretions. However, more often than not, these claims are being submitted with one general ICD-10 code: H04.123, “dry eye syndrome of bilateral lacrimal glands.” In order to create a larger return, it’s important to realize other factors that you may use to increase your level of appropriate coding.
Dry Eye Syndrome is an incredibly common problem among patients of all ages. Doctors regularly treat and prescribe patients complaining of a burning, gritty feeling in their eyes, which can be caused by a reduction of lacrimal secretions. However, more often than not, these claims are being submitted with one general ICD-10 code: H04.123, “dry eye syndrome of bilateral lacrimal glands.” In order to create a larger return, it’s important to realize other factors that you may use to increase your level of appropriate coding.
While H04.123 is the most commonly used code for patients complaining of dry eye, there are actually at least 40 billable codes for these symptoms, ranging from dry eye syndrome, to corneal erosion, to keratoconjunctivitis. One helpful list of these codes may be found here. Simply by using H04.123, you are limiting yourself to coding no greater than 992X3, which leads to limited reimbursement. By educating yourself on other codes that justify higher CPT levels, you will increase reimbursement.
When treating a patient complaining of symptoms related to dry eye syndrome, it is important to review their entire medical history. It is widely known that medical conditions such as lupus, Rheumatoid arthritis, Sjögren’s Syndrome, and thyroid issues are more likely to also have dry eye disease. Patients with a diagnosis of diabetes or glaucoma also tend to be at a greater risk of dry eye. When coding for visits with such patients, pay attention to the ICD 10 codes you document. To bill a 992X4 CPT, the AMA requires you to meet at least 1 out of 3 of the following categories:
● Tests, documents, or independent historian(s)
○ Any combination of 3 from the following:
⎻ Review of prior external note(s) from each unique source
⎼ Review of the result(s) of each unique test
⎻ Ordering of each unique test
⎻ Assessment requiring an independent historian(s)
You’re leaving reimbursements on the table with improper coding. You’re also leaving your patients in the lurch, with insurance plans only covering specific dry eye codes and potentially leaving patients to pay out-of-pocket for their eye drops. Coding parameters change and can be confusing. If you want to make sure your billing and coding department is running properly hire a consultant. They can look over your books and see what you’re missing out on. Some practices even outsource their billing and coding entirely, delegating this incredibly important task to outside professionals.
 While it is important to document any data collected from the patient or the above categories, also remember to properly document time spent with your dry eye patient. For a 992X4, a total time of 30-39 minutes for established patients, or 45-59 minutes for new patients, must be documented in the medical record.
While it is important to document any data collected from the patient or the above categories, also remember to properly document time spent with your dry eye patient. For a 992X4, a total time of 30-39 minutes for established patients, or 45-59 minutes for new patients, must be documented in the medical record.
While billing a 99212 for an established patient who presents with gritty, itchy eyes, and is found to have dry eye syndrome of bilateral lacrimal glands is not incorrect, it leaves you less opportunity to build on that diagnosis to determine any additional or underlying causes, such as punctate or superficial keratitis, or something as complex as Sicca syndrome with keratoconjunctivitis (M35.01). Instead of simply choosing the most simplistic code, you are able to document a higher level of care, which can benefit both your patient and your bottom line.
While it is important to document any data collected from the patient or the above categories, also remember to properly document time spent with your dry eye patient. For a 992X4, a total time of 30-39 minutes for established patients, or 45-59 minutes for new patients, must be documented in the medical record.
While billing a 99212 for an established patient who presents with gritty, itchy eyes, and is found to have dry eye syndrome of bilateral lacrimal glands is not incorrect, it leaves you less opportunity to build on that diagnosis to determine any additional or underlying causes, such as punctate or superficial keratitis, or something as complex as Sicca syndrome with keratoconjunctivitis (M35.01). Instead of simply choosing the most simplistic code, you are able to document a higher level of care, which can benefit both your patient and your bottom line.